When we think about gut health, we tend to focus on food. “Food is just one part of it, and I think people either engage in food-blaming, or think they need to eat all these expensive things,” says nutritional therapist Eve Kalinik. “But actually, there are other things, such as sleep, exercise and how we’re eating, that are just as important.” The good news is they’re easy, low cost, and you can start right away. Here, then, are 12 expert tips on how to get and maintain good gut health.
Eat at least 30 different plants a week
A lot of diet advice, says Kirsten Jackson, known as the IBS Dietitian, is focused on restriction – reducing calories and fat. For gut health, she says, think about additions to your diet, especially plants. We should aim to eat at least 30 different plants a week. “By ‘plants’, even coffee would count as one, a spice would count as another.” Grains too, so don’t just stick to (wheat-based) bread and pasta all week – add others such as barley, rice and quinoa. Add herbs to dishes and eat nuts as snacks and you’ll soon get up to 30. “It’s not necessarily just fruit and veg,” says Jackson.
Choose powerful polyphenols
“Phytochemicals is the sciencey name, but they are essentially a type of plant chemical that we get in a lot of our plant-based foods that are thought to boost our health that bit further,” says Annie Coombes, dietitian and clinical director of The Gut Health Clinic. “One of the most well-studied classes of phytochemicals are the polyphenols. Most of them – about 90% – skip through your small intestine to join our community of gut microbes in the large intestine, where we think the magic happens. Our microbes then help to transform them into chemicals that can be absorbed and have even been linked with reducing the risk of cancer, as well as better heart and mental health.” Coombes recommends adding polyphenol-rich foods to your diet, such as coffee, green tea, berries, flaxseeds, hazelnuts, extra virgin olive oil, broccoli, red onion, and herbs and spices, such as cinnamon, ginger and mint, though there are many others including, happily, red wine and dark chocolate. Aim for 30 different plant sources a week and you’ll probably get polyphenols without thinking about it.
Get enough fibre
Ideally, at least 30g of fibre a day, says Jackson. “That has been shown to reduce the risk of inflammatory conditions, cancer, heart disease and diabetes. It’s about looking at every meal, and making sure that it is very much plant-based.” It doesn’t have to be vegan, she says, “but aim to have, in every meal, some sort of whole grain, so something like wholemeal bread, quinoa or brown pasta, and then half of the plate to be vegetables.” Jackson suggests a couple of vegan meals a week, “just to get as much fibre as possible”.
Learn to love new plants
Get creative and adventurous. Coombes recommends using dips and seasonings, and “being versatile with your cooking methods means a variety of flavours can be experienced as they all create different ones. To maximise nutrient retention try poaching and boiling; leaving the skin on can also add different texture and added fibre.” Making a batch of roast vegetables at the weekend “means you can add them into your weekly meals with ease”. Use as much of the plant as possible – it saves waste, money, adds more flavour and fibre. Some people swear by eating apples, stem and core and all, but it’s not for Coombes – she prefers extras such as cauliflower leaves and broccoli stems.
Avoid gut-harming foods
Kalinik says ultra-processed foods have a negative effect on the gut microbiome. “Ultra-processing, in a nutshell, refers to foods that have a lot of added chemicals, such as additives, preservatives, emulsifiers, and artificial sweeteners – basically ingredients that you wouldn’t recognise as ‘food’. There are now studies showing that these foods affect both the diversity and composition of the gut microbiome, meaning that we see an increase in less friendly microbes and a decrease in those that are considered beneficial.” These types of foods also tend to contain little or no fibre. She cautions against fixating “on one aspect” and says it’s hard to avoid UPFs completely, “but where we can minimise [consumption] the better for us and [our] gut microbiome”. Coombes adds that too much alcohol can cause inflammation in our gut and “lead to [its] lining becoming more permeable, or leaky. This means that we are more likely to experience gut symptoms after eating, or develop intolerances. In terms of the impact on gut microbes, there’s some evidence that chronic alcohol consumption can cause an imbalance and may be associated with increased gastrointestinal inflammation. The good news is this isn’t permanent, and a reduction in alcohol and increased dietary diversity can restore the balance.” If you do choose to drink, it’s about moderation, she says, and some alcoholic drinks, such as red wine, have some “gut microbiota benefits in small amounts, as it contains polyphenols and has been associated with greater microbial diversity”.
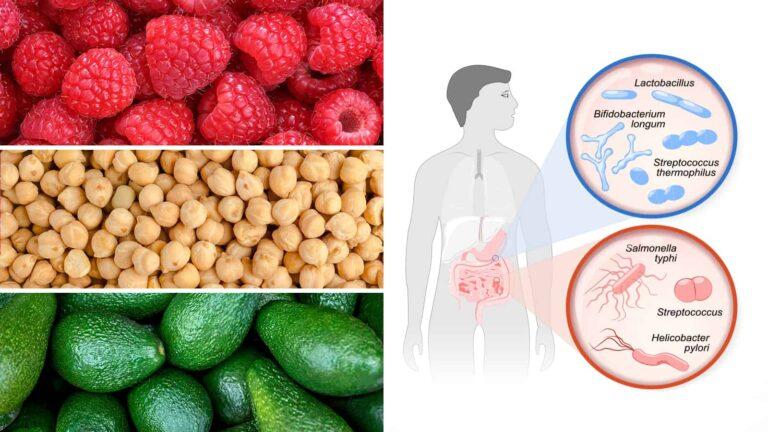
Get probiotics from fermented foods
Fermented foods contain probiotics, the “good” bacteria. Sources are sauerkraut, kimchi, kefir, live yoghurt and some cheeses. Basic supermarket cheddar will have some probiotic benefits, but unpasteurised cheese is better (it hasn’t been through the heat process which kills bacteria) “because you get more diversity and strains of bacteria in there. Fresh cheeses that are not fermented, like mozzarella, don’t have probiotics in them, so it’s the harder cheeses you’re looking for.” It’s about cumulative benefits, says Kalinik, author of Happy Gut, Happy Mind, “not just having sauerkraut once in a blue moon.” A “condiment-sized serving” of something like sauerkraut or kimchi will do, and larger portions of yoghurt or cheese, she says – and regular consumption is key. “We don’t know how much of these things actually stay in the gut. They do have a transitionary effect and that’s why regular consumption is important. It has that positive benefit as those beneficial bacteria are moving through the gut.”
… and prebiotics
If probiotics contain the bacteria itself, prebiotics “are the food that feeds our gut microbes – think fertiliser,” says Coombes. “The main prebiotics include inulin, fructooligosaccharides (FOS) and galactooligosaccharides (GOS), which can be found in more than 35,000 plant species. They are linked to supporting our immune system, bone and skin health, as well as improving blood sugar control and regulating appetite.” Supplements are not necessary, says Coombes. “For the majority of people, we can take advantage of the naturally occurring prebiotics in food to help feed our gut microbiota.” Good sources include almonds and cashews to snack on. “Add some prunes, dates or dried apricots to natural live yoghurt and try to include more grains and legumes in your day, so switch rice or pasta to freekeh, quinoa, buckwheat or spelt or add legumes into sauces.” Good vegetable sources include artichokes, asparagus, beetroot, chicory, fennel, garlic and leeks, as well as legumes. Add a handful of chickpeas to sauces and curries, “or try in any of your favourite recipes – they can even be hidden in muffins”.
Take time to eat
Not many of us do this, says Jackson. “We’re always on the go and this can mean that we don’t chew foods fully.” We concentrate on the food we’re putting in our gut, “but digestion starts before we put the food in our mouth – when we look at food, we’re starting to produce saliva. Then chewing it gives the food a bigger surface area, so when it does meet the digestive enzymes further down, it can get broken down a lot easier.” With bigger chunks, “they’ve got more work to do. That might mean there’s food going into parts of the gut undigested, and that can lead to fluid being brought in, excess gas being produced.” How do you know you’ve chewed enough? “Probably looking at consistency. If it’s more like a paste, then you’re ready to swallow.” Take a proper lunch break and eat slowly, adds Coombes. “Research shows if you take that break, you actually get more done in the afternoon and in less time.” Eat with other people if you can (and want to). “Eating – and many of the associated health benefits – is about community, culture and experiences, as well as nutrients.”
Practise mindfulness
“We know that stress can be one of the major triggers in gut-related symptoms,” says Kalinik. “Include a daily mindful practice, which could be breathing exercises or meditation, because that helps to support the gut-brain connection. It’s a bidirectional relationship. The gut talks to the brain, the brain talks to the gut, and it does it through this massive highway called the vagus nerve. So when you do the deep breathing that forms the basis of a lot of practices like yoga and tai chi, what you’re doing is essentially soothing that vagus nerve.” It helps move the body, she says, from the sympathetic (fight or flight) state, to the parasympathetic (rest and digest), “which is optimum for gut health. If we’re chronically in fight or flight, that’s going to impact on things like motility, so movement through the gut, which can change people’s bowel movements, either making them more urgent or constipated. The production of stress hormones, such as cortisol, can directly impact the composition of the bugs in our gut as well, which then exacerbates any gut issues.” Five minutes every day is better than doing it once in a while and meditating for an hour. “It doesn’t need to be laborious, it’s the cumulative benefits that add up over a long time.”
Get moving
Move as much as you can throughout the day. Doing an hour of intense exercise, but then sitting at a desk for the rest of the day, isn’t going to be great for digestion. “Simple things like getting out during a lunch break and trying to walk for 20 minutes can really help,” says Jackson. “We know that movement outside especially will help the microbiome as well, because you’re coming into contact with more microbes.” Moving can help you feel less bloated. “We don’t know exactly why, but it’s probably because when we’re moving we actually release small amounts of gas, because bloating typically comes from gas, even maybe produced in normal digestion, but it’s just sitting in the gut so it makes us feel uncomfortable.” There’s also the mental health benefits. “There’s probably an element where the brain is being impacted beneficially and that then has another impact on the gut.”
Fast overnight
That’s enough food for now. “We need adequate fasting periods between meals, because we have microbes that help us digest and absorb our food, and then we have a different set of microbes that essentially do a kind of clean-up operation and manage inflammation – and that type of thing happens in a fasted state,” says Kalinik. “Broadly speaking, have a 12-hour overnight fast, so not eating from say, 8pm to 8am, and also allowing periods between your meals.” Sleep also has a huge role to play in gut health, says Kalinik, so you should prioritise good sleep habits. “Even one night of disrupted sleep, we know, has an impact on pretty much every system in the body, including the gut, and can even shift the composition of the microbiome.”
Keep at it
“A lot of us go from one extreme to the other,” says Kalinik, whereas good gut health is “about consistency and patterns over time.” Don’t let an occasional week of excess or processed food derail you entirely. “It’s really not going to have that big an effect,” she says. Just get back to the good gut practices and try to make them part of your life.
This content was originally published here.