We hear so much about nurturing the microbes in our gut, but there’s another important ecosystem that rarely rates a mention: the vaginal microbiome. But when it’s thrown out of balance, women’s health can suffer – a higher risk of preterm birth, miscarriage, STIs, pelvic inflammatory disease, thrush and UTIs are all linked to a disrupted vaginal microbiome.
The first thing to know is that the vagina has a star defender – a type of bacteria called lactobacilli that produce lactic acid, a killer of unwanted microbes.
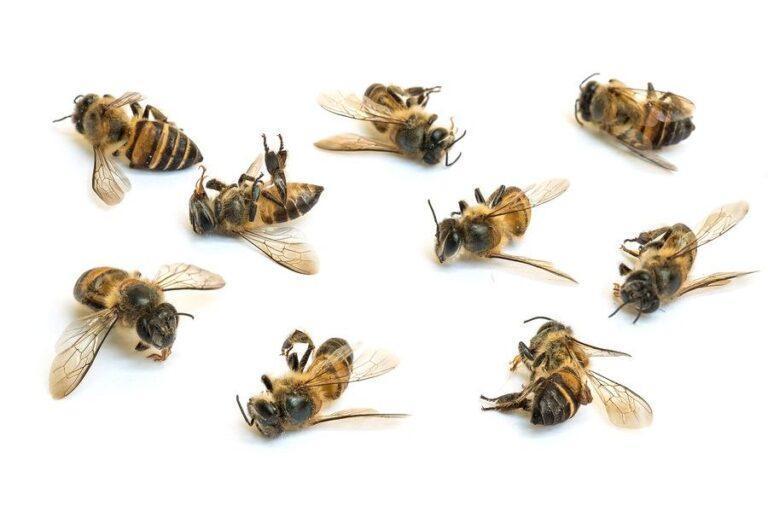
Leave the feminine hygiene products and let nature play its role.Credit:iStock
“When lactobacilli are dominant, the vagina can fight off infection, but if something alters the balance it’s less able to defend itself and this can lead to bacterial vaginosis, a common infection often mistaken for thrush,” says Dr Terri Foran, a sexual health physician and conjoint senior lecturer at the School of Women’s and Children’s Health at the University of NSW.
About 30 per cent of women will have BV at some time in their lives, Foran says.
Antibiotics, menstruation, sex, menopause, even having an IUD inserted can all cause lactobacilli numbers to fall, but the factors most strongly linked to a high risk of BV include sex with a new partner, having a female sexual partner, not using condoms – and cleaning inside the vagina with water, soap or douching.
There are also question marks over whether feminine hygiene products marketed to clean or “freshen” the vagina can also disrupt lactobacilli. Although 2018 research from Canada’s University of Guelph linked the use of some products to a higher risk of problems like BV, thrush, STIs and UTIs, scientists say more research is needed to understand their effects.
Either way, Foran’s advice is to leave them on the shelf. “The vagina is self-cleaning – it can look after itself,” she says.
Symptoms of BV include a “fishy” odour and increased discharge.
“More than half of women treated for BV with antibiotics will get a recurrence within six months,” says Dr Catriona Bradshaw, a sexual health physician and professor at Monash University. She believes BV can be sexually transmitted, and that successful treatment depends on treating not just women but their sexual partners too – studies have found that the microbes responsible for BV are also carried by men, especially uncircumcised men.
“If you only treat women, not men, you won’t have high levels of cure. We know condoms reduce the risk of BV – and if that’s not evidence, I don’t know what is,” says Bradshaw, who’s been involved in research to see if treating both women and their male partners prevents BV recurring. The trial treated both partners with oral antibiotics, and treated men with an antibiotic cream for the penis.
Hope for a cure?
If the treatment works – and she’s confident it will – Bradshaw believes it could offer women with BV the first real opportunity for a cure in decades for a problem that’s more than just an inconvenience.
This content was originally published here.














![Healthy Vegetable Soup Recipe [Detox Soup] - The Healthy Maven](https://thehealthandwellnesscrier.com/wp-content/uploads/2023/01/Healthy-Vegetable-Soup-Recipe-Detox-Soup-The-Healthy-Maven.jpg)