Generally speaking, the likelihood that a person will develop a chronic disease increases as they get older. Advanced age is among the top five risk factors for heart disease, type 2 diabetes, obesity, and arthritis, just to name a few.
Migraine, however, is a notable exception: Many people (fortunately) age out of the condition over time.
Migraine typically starts in childhood or adolescence in both boys and girls. During puberty and the teenage years, the number of girls who develop migraine increases at a higher rate than for boys, and by adulthood, migraine is about three times more common in women than in men, research published in Neurological Sciences in 2020 has shown.
“The peak prevalence — the age at which migraine is most common — in both men and women is at about age 40,” says Gretchen Tietjen, MD, a professor emerita of neurology at the University of Toledo in Ohio and an expert in migraine in older adults. “At that point, it tapers off in both sexes,” Dr. Tietjen says.
How Many Older Adults Have Migraine?
Migraine affects about 1 in 10 older adults each year, and it’s the second most common headache disorder (after tension headache) in older adults, according to a review published in April 2022 in Current Pain and Headache Reports.
Many of the people who have migraine after age 60 are those who have had attacks throughout their lifetime, but it is possible — though less common — to develop migraine as an older adult, according to the authors of the review.
According to Tietjen, the people who tend to continue to have migraine later in life are those who first developed migraine as a child or teen.
“If people do have migraine that continues to persist into older age, frequently the attacks are less often, and the symptoms are less severe, so that’s one good thing that can happen with age,” says Tietjen. But unfortunately, there are some people who are older — even into their eighties — who still have regular attacks, she says.
How Does Migraine Change After 60?
Migraine characteristics in older adults can differ from those in younger people.
It’s likely that a combination of factors contribute to migraine triggers, frequency, and symptoms, and those can change over time, explains Nina Riggins, MD, PhD, a headache specialist and the director of the headache and traumatic brain injury center at UC San Diego Health in California.
When it comes to triggers, stress and hormones are two of the biggest migraine triggers in people age 40 and younger, according to the American Headache Society.
But for people in their fifties and sixties, pain, alcohol, and smoking are more likely to bring on an attack.
In addition to migraine symptoms being less severe, they can also be different in older age, says Dr. Riggins.
For example, migraine attacks may come without light or sound sensitivity, and there may be fewer cranial autonomic symptoms, such as nasal congestion, ear fullness, ptosis, and tearing of the eye, she says.
At least one study has also shown that it’s not uncommon for older adults to experience visual aura without associated headache, and that this often begins after age 50. Since visual aura and stroke symptoms can be similar, adults with new visual aura should inform their doctor about this symptom.
“There are also studies that show that headache can have tendency to be more bilateral (on both sides of the head),” Riggins says. Typically, migraine causes pain on one side of the head.
For Women, Migraine Usually Improves After Menopause
The majority of women of childbearing age with migraine report a connection between their menstrual cycle and migraine attacks, according to Cleveland Clinic.
“After menopause, migraine often improves, especially in women who have menstrual migraine,” says Tietjen. But there are still a significant number of women who continue to have attacks, she adds.
“The best explanation for why more women have migraine than men do is reproductive hormones,” she says. In a normal menstrual cycle, fluctuating levels of estrogen and progesterone can trigger menstrual migraines.
“But even after menopause, more women than men continue to have migraine, so it has to be something besides estrogen causing more migraine in women,” says Tietjen.
Medication Interactions and Side Effects in Older Adults
For a number of reasons, older adults with migraine should review their migraine prevention and treatment plan with their healthcare provider.
One reason is that as a person gets older, says Tietjen, the effect of certain medications on the body may change.
“What might have been an appropriate dose of a medication when you were younger may cause issues later in life because you metabolize it differently. You can’t think that a drug or a certain dose of a drug is going to be safe throughout your entire life just because it was safe when you were younger,” she says.
A person may also develop contraindications — or reasons not to take certain drugs over time.
In particular, the use of medications that can narrow blood vessels, such as triptans and ergots, may need to be reevaluated in older adults, even if they have been successfully used to manage migraine in the past, says Tietjen. These drugs are contraindicated in people who have coronary artery disease, peripheral vascular disease, uncontrolled high blood pressure, or a history of heart attack.
“There are now newer medications that can be a good option to replace these medications, if necessary,” Tietjen says.
Drug interactions are another concern in older adults, who may be on several different medications for other chronic conditions besides migraine.
“Medication interactions and medication side effects are very important to discuss and follow with older adults,” says Riggins.
Tests to monitor liver function should be done in those taking acetaminophen, she says, and in people taking nonsteroidal anti-inflammatory medications (NSAIDs), kidney and liver function should be monitored, as well as any adverse effects on the heart and stomach.
For individuals with multiple health problems, it’s important for primary care providers and specialists to coordinate with one another to create a treatment plan that is safe and effective.
Newer Medications May Help Manage Migraine in Older Adults
“CGRP-blocking medications called gepants can be used in older adults with success, when appropriate,” says Riggins. Gepants work by blocking the action of CGRP, a protein in the brain and nervous system involved in the transmission of pain.
These medications include the oral medicines ubrogepant (Ubrelvy), rimegepant (Nurtec ODT), and atogepant (Qulipta). Ubrelvy treats acute migraine attacks, Qulipta is used preventively, and Nurtec can be used for both.
“These medications are thought to be relatively safe, even in a person who has cardiac disease,” says Tietjen.
Another advantage of the CGRP blockers is that they don’t carry a risk for medication-overuse headache (MOH), a type of chronic daily headache caused by overusing acute headache medications, as well as some other drugs.
In a study of migraine in people 65 and older, researchers found that 30 percent of the subjects had probable medication overuse. Of those people overusing medications, about 3 in 10 overused triptans and 7 in 10 overused combination analgesics (pain relievers).
Lasmiditan (Reyvow) is another type of new drug that works similarly to triptans but doesn’t cause vasoconstriction (narrowing of blood vessels). “It’s thought that this drug may be a safe drug to use acutely for cardiac patients,” says Tietjen.
An analysis of data from three studies of lasmiditan evaluated the safety of the drug in treating migraine in elderly people, with a special emphasis on cardiovascular-related issues, because heart conditions are more common in older people. The study found no excess adverse events occurring after the start of treatment, nor increased “cardiovascular safety signals” in the elderly population.
Other Options for Managing Migraine in People Over 60
There are several procedures used in the treatment of migraine that can be good options for older adults, says Riggins. These include:
Another treatment option that’s safe for older adults is neuromodulation, in which electrical or magnetic pulses are delivered to specific nerves or areas of the brain to either prevent migraine attacks or reduce the severity of symptoms during attacks. Several self-administered neuromodulation devices are available in the United States.
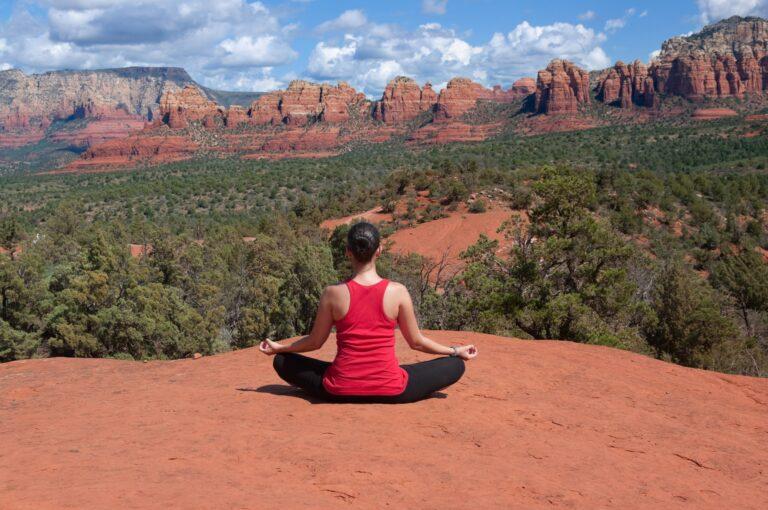
And for people of any age, lifestyle measures, such as following a healthy diet and getting regular exercise, and behavioral modalities such as biofeedback and mindfulness, can have a meaningful effect on reducing migraine frequency and severity.
This content was originally published here.